The UB-04 claim form is a vital tool in healthcare billing. It is used by hospitals to bill insurance companies for services provided. This standardized form ensures accurate billing and reimbursement for healthcare services.
Understanding the UB-04 form is crucial for healthcare professionals and patients alike. It helps in navigating the complex world of medical billing.
The form includes detailed fields for patient information, insurance details, and service codes. Each field has specific instructions to ensure accuracy.
Errors in the form can lead to claim denials or payment delays. Therefore, proper completion is essential for smooth billing processes.
This guide will provide a comprehensive overview of the UB-04 claim form, its purpose, and usage.
UB-04 Claim Form Overview
The UB-04 claim form, also known as the CMS-1450, is fundamental for institutional billing in healthcare. It serves as a tool for hospitals and similar providers to communicate billing information to insurers efficiently.
Primarily, the form is utilized by various healthcare institutions, including hospitals, nursing facilities, and home health agencies. These providers use the UB-04 form to document inpatient and outpatient services rendered to patients.
The National Uniform Billing Committee (NUBC) maintains the integrity and updates of the UB-04 form. This ensures it aligns with current healthcare billing standards. Over 80 fields populate the form, each demanding specific details to avoid discrepancies.
Key components of the UB-04 form include:
- Patient demographics
- Insurance information
- Revenue codes
- Service and condition codes
The UB-04 simplifies complex billing processes, ensuring standardization across the board. Its meticulous design enables accurate data capture and seamless transmission between healthcare providers and insurance companies. This efficiency underpins the financial stability of many health institutions.
History and Purpose of the UB-04 Form
The UB-04 form has roots deeply anchored in healthcare billing history. It replaced the outdated UB-92 form in 2007. This transition aimed to streamline billing processes and enhance compatibility with modern billing systems.
The main goal of the UB-04 form is to standardize billing for healthcare institutions. It ensures that claims submitted to insurers are uniform, improving processing times and reducing errors. This standardized format facilitates communication between providers and insurers.
Healthcare facilities rely on the UB-04 form to detail services provided to patients, which is pivotal for accurate billing. This form is essential for documenting both inpatient and outpatient services, acting as a bridge between service delivery and financial reimbursement.
Critical purposes of the UB-04 form include:
- Enhanced billing accuracy
- Faster claim processing
- Uniform communication with insurance carriers
This form plays a key role in sustaining financial health for service providers, ensuring that they receive timely payments for their services.
Who Uses the UB-04 Claim Form?
The UB-04 claim form is utilized by various healthcare providers. Institutional providers like hospitals, nursing facilities, and home health agencies commonly use it.
These providers use the form to bill insurers, including Medicare and Medicaid. It is also essential for billing private insurance companies.
The form is not just for institutional use. It’s crucial for medical billing specialists and hospital billing departments. They rely on it to ensure accurate claim submissions and financial management.
Key users of the UB-04 form include:
- Hospitals
- Nursing facilities
- Home health agencies
- Medical billing specialists
Understanding the form is not just vital for health institutions. Patients could benefit from understanding it to verify their medical bills.

Proper usage of the UB-04 form helps maintain financial health in healthcare systems. It ensures transparency and consistent communication with payers.
Key Sections and Fields on the UB-04 Form
The UB-04 form has many fields designed to capture essential billing details. It includes over 80 fields that serve different purposes, covering everything from patient details to specific service codes.
Each field on the form demands accuracy to prevent errors in billing. These fields are grouped into sections that guide users through the information required for claims.
A critical section involves patient demographics. This part gathers necessary information about the patient’s identity and contact details.
Another integral section covers service codes. These codes categorize treatments and procedures, ensuring billing consistency.
Commonly featured fields on the UB-04 form include:
- Patient demographics
- Admission and discharge details
- Revenue and service codes
- Condition and diagnosis codes
Hospitals often use these sections to communicate accurately with insurers about services provided. This format ensures that institutions comply with healthcare regulations.
Correctly filling these sections helps avoid claim denials. It also streamlines the billing process, resulting in quicker reimbursements.

UB-04 Billing Process: Step-by-Step
The UB-04 billing process is crucial for hospitals and insurers. This standardized form simplifies the claims process by ensuring all necessary information is present.
The first step in the billing process is data entry. Hospitals gather patient information, including demographics and insurance details, and input these into the form accurately.
Next, the form must include service and revenue codes. These codes specify the procedures and treatments that were provided to the patient.
After the form is filled, it undergoes a review for completeness and accuracy. This step reduces the risk of errors, which could lead to claim denials.
Finally, the form is submitted to the insurance company, typically electronically. This method speeds up processing times and facilitates smoother communication.
Key steps in the process include:
- Gathering patient information
- Inputting service and revenue codes
- Reviewing for accuracy
- Submitting electronically
Each step is vital for ensuring timely and accurate reimbursement.

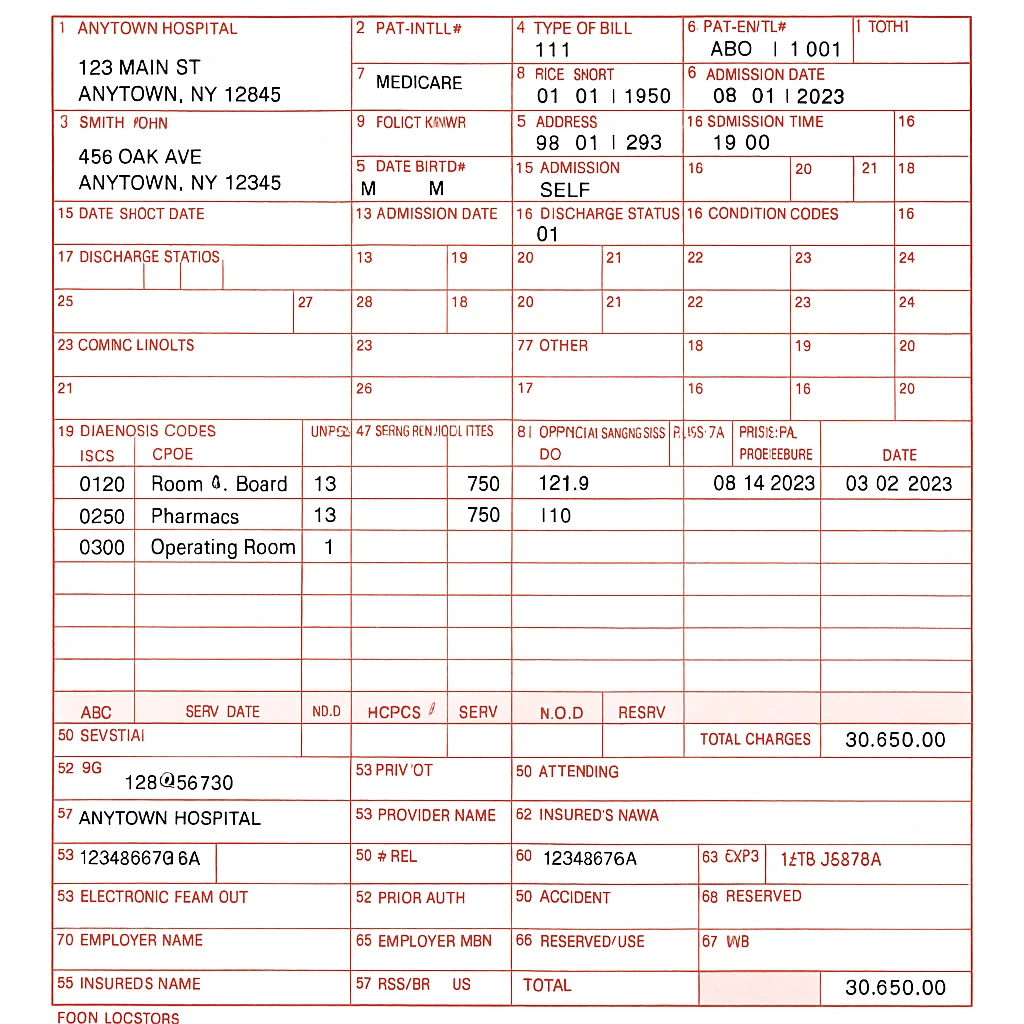
UB-04 Claim Form Example and Sample
A UB-04 claim form sample can be very useful to healthcare providers. It offers guidance on how the form should be completed. Seeing a filled-out example can prevent common errors and ensure accuracy.
A typical UB-04 form includes over 80 fields. Examples of these fields are patient demographics, condition codes, and revenue codes. Each field has a specific purpose, such as identifying the services provided or the institution submitting the claim.
Reviewing a UB-04 claim form example can also highlight the essential elements to include. This includes proper coding and detailed patient information, which are crucial for claim approval.
Features of a sample form might include:
- Patient name and insurance details
- Procedure and diagnosis codes
- Date of service and facility information
This example form serves as a practical tool for understanding the structure and requirements of UB-04 billing.

UB-04 Instructions: How to Fill Out the Form
Filling out the UB-04 form correctly is essential for smooth billing. Each field requires specific information. Understanding these requirements can prevent claim denials.
Start with patient details, such as name and address. Next, include insurance information and policy number. Accurate data entry is crucial to avoid errors.
Pay special attention to coding. Use correct ICD-10 and CPT codes for diagnoses and procedures. Mistakes here can lead to delays in processing.
Additionally, follow specific instructions for completing each field. Healthcare facilities should train staff on current guidelines to ensure compliance.
Key steps to complete the form include:
- Entering patient and provider information
- Completing insurance and payer details
- Adding correct service and diagnosis codes
Following these instructions ensures the UB-04 form is both accurate and efficient.
Common Errors and How to Avoid Them
Errors on the UB-04 form can delay payments. They might even result in denials. Recognizing common mistakes is the first step to prevention.
Frequent errors include incorrect codes and missing signatures. Also, inaccurate patient information often causes issues. Prevent these by double-checking each section.
Implement a review process to catch mistakes. Trained staff should verify entries. Regular updates on coding changes can also minimize errors.
Key points to avoid errors:
- Verify patient details and signatures
- Use current ICD-10 and CPT codes
- Cross-check each section before submission
How to Get a UB-04 Form from a Hospital (Online and Offline)
Obtaining a UB-04 claim form is straightforward. Hospitals often have these forms readily available. They can be accessed both online and offline.
To get a form online, visit your hospital’s website or the NUBC site. Often, hospitals provide downloadable copies. This allows for easy printing and completion.
For offline access, contact the hospital’s billing department. They can provide physical forms. Typically, these are available at the hospital’s main office or billing section.
Ways to obtain the UB-04 form:
- Visit the hospital’s website for online forms
- Contact the billing department for offline forms
- Check the NUBC website for downloadable options

UB-04 vs. CMS-1500: Key Differences
The UB-04 and CMS-1500 are both essential forms. However, they serve distinct purposes in medical billing. Understanding their differences is crucial for accurate billing.
The UB-04 form is primarily used by institutional providers. These include hospitals and nursing facilities. In contrast, the CMS-1500 is used by individual healthcare providers like physicians.
Key differences include:
- Usage: UB-04 for institutions, CMS-1500 for individuals
- Providers: UB-04 for hospitals, CMS-1500 for doctors
- Service Scope: UB-04 for inpatient, CMS-1500 for outpatient services
Why Understanding the UB-04 Form Matters
Understanding the UB-04 form is essential for successful medical billing. It’s a vital tool that impacts revenue and compliance. Proper knowledge reduces billing errors and improves reimbursement rates.
Key reasons why it matters include:
- Accuracy: Ensures correct claim submissions
- Compliance: Aligns with healthcare regulations
- Efficiency: Speeds up billing processes
Mastering this form enhances the financial stability of healthcare institutions by reducing the risk of audits.
Conclusion and Key Takeaways
The UB-04 claim form is a cornerstone in healthcare billing. Proper understanding of its sections and usage maximizes reimbursement and ensures regulatory compliance. This efficiency is crucial for the financial health of medical facilities.
Key takeaways include:
- Comprehensive Understanding: Essential for billing success
- Error Reduction: Crucial for avoiding claim denials
- Financial Impact: Directly influences cash flow
By mastering the UB-04 form, healthcare providers enhance both revenue management and operational efficiency.






Comments are closed