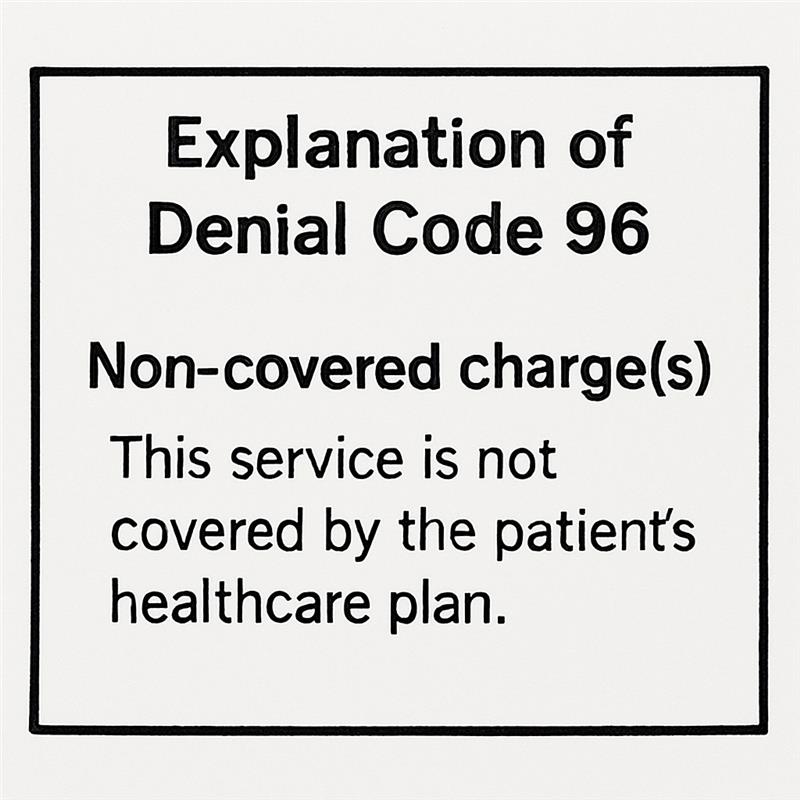
Navigating insurance claim issues can be daunting. Denial Code 96 is a common hurdle in this process. It signifies non-covered charges, often leaving healthcare providers puzzled. Understanding this code is crucial for effective resolution.
Denial Code 96 can stem from various claim denial reasons. These include services not covered by the patient’s plan or deemed unnecessary. Knowing the specific reason is key to addressing the issue.
Proper documentation and coding are vital to prevent this denial. Errors in billing or coding can trigger Denial Code 96. Ensuring accuracy in these areas can save time and resources.
Communication with insurance companies is essential. Clarifying the denial reason can lead to a quicker resolution. This guide will explore Denial Code 96, offering insights and solutions.
By understanding and addressing Denial Code 96, healthcare providers can improve claim acceptance rates. This article will provide a comprehensive overview and actionable steps to tackle this insurance denial code effectively.
What is Denial Code 96?
Denial Code 96 is a common rejection code used by insurance companies. It indicates that certain charges are not covered under a patient’s insurance plan. This denial code is part of the CO (Contractual Obligation) group, emphasizing non-covered services.
This code plays a crucial role in the billing process. It’s important to identify the reason behind this code to resolve the issue effectively. Often, Denial Code 96 is linked to services deemed not medically necessary or experimental.
Understanding the exact context of Denial Code 96 can help in managing billing efficiently. Consider the following possible scenarios leading to this denial:
- Services outside the coverage period
- Procedures not approved by insurance
- Charges exceeding policy limits
- Lack of pre-authorization for services
Efficient management of Denial Code 96 involves verifying patient eligibility and staying informed about insurance policies. Embracing technology can also aid in understanding and processing these denials more effectively.
Recognizing the importance of Denial Code 96 can significantly impact revenue. By decoding this denial, healthcare providers can streamline their billing processes, leading to better financial outcomes.
CO 96 vs PR 96: Understanding the Differences
Denial codes CO 96 and PR 96 may appear similar but have different implications for billing. CO 96 represents a Contractual Obligation where the insurer is not liable for the charges. This means services provided are not covered, and no payment is due from the insurance company. It often results from issues like coverage limits or uncovered services.
On the other hand, PR 96 stands for Patient Responsibility. This code indicates that the patient is liable for the uncovered expenses. It highlights scenarios where patients must pay out-of-pocket, perhaps for non-covered procedures or deductibles.
Understanding these differences is vital for effective billing and collections:
- CO 96: Insurance not liable for charges
- PR 96: Patient liable for certain charges
- Different billing routes for CO and PR codes
Healthcare providers must differentiate between these codes to handle claims efficiently. Proper coding ensures accurate medical billing and minimizes confusion for patients.
By grasping the nuances between CO and PR codes, billing staff can avoid processing errors, benefiting both the healthcare provider and the patient.
Common Reasons for Denial Code 96
Denial Code 96 is often linked to non-covered services. Insurance plans have specific terms dictating which services are covered. When services fall outside these parameters, denial is likely.
Billing errors contribute significantly to Denial Code 96. This occurs when billing details are incorrect or missing. Such errors can complicate the claim process, leading to delays and denials.
Another common issue is lack of medical necessity. Insurers often deny claims if they believe a service is not medically essential. This determination is based on guidelines provided by the insurance policy.
Additionally, inadequate pre-authorization is a frequent denial trigger. Many insurers require pre-approval for certain procedures. Failure to obtain this can result in denial.
Finally, technical issues like incorrect coding or submission errors can lead to Denial Code 96. It’s crucial to ensure that all codes are accurate and submissions timely.
To summarize, common reasons include:
- Non-covered services
- Billing errors
- Lack of medical necessity
- Inadequate pre-authorization
- Technical issues like incorrect coding
Understanding these reasons can help in addressing and preventing future denials.
By recognizing these factors, healthcare providers can implement measures to reduce claim denials. Preventing such issues ultimately improves efficiency and revenue flow.
How Denial Code 96 Impacts Healthcare Providers
Denial Code 96 can significantly affect a healthcare provider’s cash flow. Non-covered charges mean providers might not receive full payment for services. This can create financial strains on their operations and resources.
Moreover, handling denied claims requires additional time and effort. Staff must investigate, correct, and resubmit claims. This increases administrative workload, diverting attention from patient care and other vital tasks.
Repeated denials can also impact the provider’s relationship with patients. Patients may become frustrated with potential billing issues. Such conflicts can hurt trust and patient satisfaction.
Key impacts include:
- Reduced cash flow
- Increased administrative workload
- Potential strain on patient relationships
Understanding these impacts helps providers prioritize effective denial management. Doing so ensures financial stability and maintains patient trust.
Step-by-Step Guide to Addressing Denial Code 96
Addressing Denial Code 96 requires a structured approach. Begin by thoroughly reviewing the denial notice from the insurance provider. Understanding the exact reason for denial is essential for a successful resolution.
Next, consult the patient’s insurance policy. This helps identify any coverage limitations or eligibility issues. Ensuring services align with the policy prevents future denials for the same reason.
Communication with the insurance company is crucial. Contact them to clarify the denial if needed. Take detailed notes of any discussions, including date, time, and representative name.
Key Action Steps:
- Review the denial notice thoroughly.
- Examine the patient’s insurance policy.
- Contact the insurer to clarify the denial.
After gathering information, correct any errors found in the initial claim. Common mistakes include incorrect billing codes or missing documentation. Make sure to address all issues before resubmitting the claim.
Ensure all necessary documentation is ready for resubmission. This may include medical records or prior authorizations. Proper documentation supports the justification of billed services.
Actionable Submissions:
- Correct any discovered errors.
- Gather supporting documentation.
- Resubmit the claim promptly.
Follow up with the insurance company after resubmission. Verify the status of the corrected claim. Timely follow-up is key to ensuring the claim gets processed without further delay.
Regularly tracking denial trends can help improve your processes. Identifying recurring issues allows for targeted training and process improvements. This proactive approach can minimize future denials.
Preventing Denial Code 96: Best Practices
Preventing Denial Code 96 involves careful preparation and attention to detail. Start by verifying patient eligibility before services are provided. Ensuring accurate information can prevent non-covered service issues.
Educating staff on common claim denial reasons is important. Regular training helps identify potential errors before submission. This proactive step can significantly reduce the occurrence of Denial Code 96.
Eligibility Verification Steps:
- Confirm patient benefits and coverage.
- Check for required authorizations.
- Verify policy effective dates.
Communication with patients plays a crucial role. Clearly explain their financial responsibilities and any limitations in coverage. This transparency can mitigate surprises and improve patient satisfaction.
Staff Training Focus Areas:
- Understanding insurance codes.
- Preventing common billing errors.
- Navigating policy limitations.
Utilize technology to your advantage. Billing software with denial management features can streamline processes. Regularly updating these tools ensures compliance with current insurance policies.
Creating a robust internal review process further helps. Performing audits of claims prior to submission can catch potential issues. This step can be key to maintaining smooth operations and reducing revenue loss.

How to Appeal a Denial Code 96 Decision
Appealing a Denial Code 96 decision requires careful preparation. Start by gathering all pertinent documentation. This includes medical records, insurance policies, and any previous correspondence with the insurer.
The next step is to understand why the claim was denied. Review the denial letter carefully to pinpoint the exact reason. This clarity will guide your appeal strategy effectively.
Crafting a compelling appeal letter is crucial. It should clearly outline why the denial should be reversed. Use detailed explanations supported by documentation to strengthen your case.
Essential Elements of an Appeal Letter:
- Patient information and claim details.
- Explanation of the service provided.
- Relevant policy information and argument for coverage.
It’s important to follow up after submitting the appeal. Regularly contact the insurance company to check the status of your case. Patience and persistence are key in navigating the appeals process.
Consider involving a professional if needed. An experienced medical billing advocate or consultant can provide valuable insights. This expertise may enhance the chances of a successful appeal.

Key Takeaways for Managing Insurance Claim Issues
Effectively managing insurance claim issues requires a strategic approach. Understanding Denial Code 96 and similar codes can prevent common mistakes. Staying informed on payer-specific guidelines is essential for success.
Implementing best practices in billing processes can reduce denial occurrences. Regular training sessions keep staff updated and aware. Proactive measures like pre-authorization and eligibility checks aid in avoiding denials.
Successful management also involves continuous improvement. Regular audits help identify and correct billing errors. Tracking denial trends enables effective response strategies.
Key Actions for Better Claim Management:
- Ensure accurate documentation and coding.
- Follow up promptly on denied claims.
- Educate patients about their insurance coverage.
Frequently Asked Questions about Denial Code 96
What does Denial Code 96 mean?
Denial Code 96 indicates non-covered charges. This occurs when services are not covered by the patient’s insurance plan or are deemed medically unnecessary.
Can Denial Code 96 be appealed?
Yes, if there’s a valid reason. Gather necessary documentation, and contact the insurer to understand their appeals process.
How can I prevent Denial Code 96?
Preventing Denial Code 96 involves several steps. Always verify patient eligibility and benefits before providing services. Accurate documentation and coding are also crucial.
What should I do if I receive a Denial Code 96?
Start by reviewing the denial notice and insurance policy. Contact the insurer for clarification. Correct any errors and resubmit with proper documentation.
Are there resources to help manage Denial Code 96?
Yes, many providers use denial management software. These tools help track denials and provide insights for resolution. Training and clear communication with insurance companies are also beneficial.






Comments are closed