Precise documentation is important to ensure that healthcare professionals are paid properly for the services they offer. CPT Code 92504 Diagnostic speech, language, voice, communication and auditory processing testing is one of the most important codes in audiology and speech-language pathology. Coding and billing this code correctly means you get paid faster and your claim will not be rejected.
This process can be eased significantly by using a medical billing company. These companies focus on assisting healthcare providers to accurately submit claims, comply with payer rules and ensure the highest reimbursement for their services. Providers should concentrate on patient care, not spend time correcting billing mistakes and fighting claim rejections for hours.
Understanding CPT Code 92504
CPT Code 92504 Behavioral Audiometry CPT Code 92504 is defined as systematic procedure for the measurement of a series of behavioral responses resulting from an instrumental signal, presented acoustically or through somatosensory stimulation. It is often used in tests of the ability of patients to process speech and language. These tests can be performed on children and adults, and are useful in the diagnosis of conditions such as speech delay, hearing loss or auditory processing disorders.
It is important to be clear about what services are covered by this code. Typical diagnostic tests with CPT 92504 are:
- Speech recognition testing
- Word recognition testing
- Auditory processing evaluation
- Language comprehension assessment
When you use this code appropriately, insurance carriers can identify the work that you do and makes certain your practice is compensated accurately.
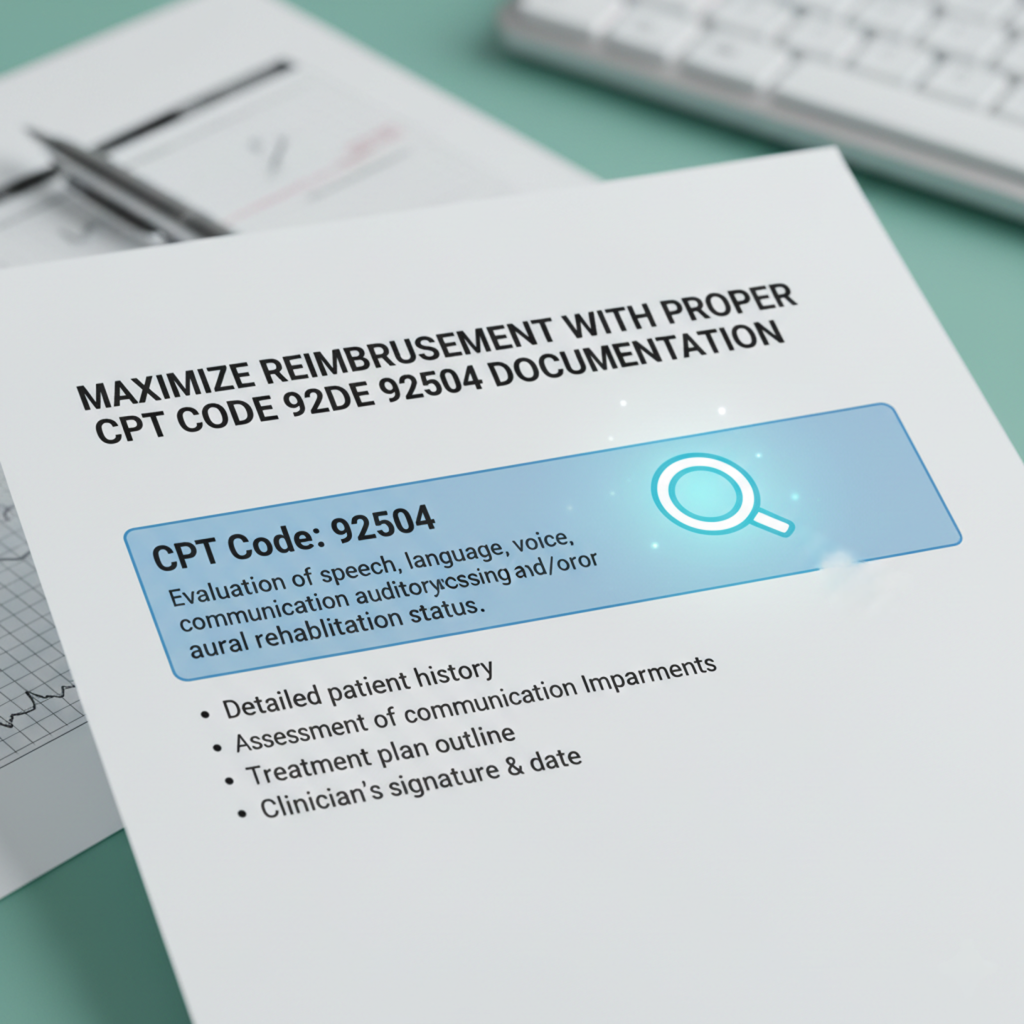
How to Notate CPT Code 92504 Properly
- Documentation Tips: The key to getting reimbursed5010 Ready EAPG Guidelines1 Proper documentation is the key to maximizing your reimbursement. Here are the important steps:
- Patient Information: Be sure to include the patient’s name, date of birth, and any pertinent past medical history. Correct information avoids delays or denial of claims.
- Indication for Testing: Indicate the reason why the test was performed. For instance, indicate the patient’s speech delay or hearing problems or any other communication difficulties.
- Specific Testing Information: Provide a list of each test that was performed at the session. Score and discuss any approaches taken. The procedure is supported by detailed documentation of its medical necessity.
- Results and Interpretation: Report the results explicitly and interpret clinically. Interpret what the findings would mean for the patient’s care.
- Provider Signature: Make sure signed and dated documentation indicating the member has been tested is available for review. Unwitnessed reports A no witness scenario is a frequent cause of claim denial.
Avoiding Common Billing Mistakes
A lot of traditional practices are not getting the money they earned because of little mistakes in documenting and coding. Some common mistakes include:
- Insufficient Documentation:Failure to include information about the tests or results may cause your claim to be returned.
- Billing with Incorrect Codes: Making use of wrong codes to bill for service outcomes can also cause audits.
- Lack of Documentation: Non-clarity regarding why the test was necessary is possible that it will be denied.
- Unsigned Declarations: Unsigned statements are generally disallowed by insurers.
How Denial Management Services Help
Despite documentation, claims can be denied. This is where denial management services come into play. These services are focused on finding out why they were denied and often correcting errors made by doctors or other companies being billed, then resubmitting claims in order to get the payment. Collaborating with denial management specialists helps medical practices recoup lost funds and alleviate the burden of managing denials in-house.
Here are some ways to decrease your claim denial rate:
- Check your codes and doc before submission
- Keeping up-to-date with payer requirements
Documentation of medical necessity for all tests_DEF_INIT echang.ecq.mcrnkingc.govt.nz?311-2 [1/6(3)]ECICAESJWOJJ../Documents… documenting medical necessity with clarity related to specific test and its sensitivity, specificity have_not been met: especially bo.
Squaring off with denied claims and not making the same mistake again
Tips to Maximize Reimbursement
Simple, Clear Language: Insurance reviewers comprehend simplicity and clarity of documentation better. Don’t use abbreviations that will confuse people.
- Check Codes: Make sure that the CPT Code 92504 matches the tests done. Refer/check payer specific guidelines for avoiding errors.
- Record Everything: Document all aspects of the assessment to substantiate the allegation. “Document everything and everything is the best way to prevent a denial.”
- Educate Your Employees: You want your administrative and clinical staff to be all on the same page when it comes to documentation/billing procedures. Efficiency and accuracy improve with regular training.
- Use EHR Templates: Providers can use Electronic Health Records (EHR) with CPT 92504 templates to ensure that all required information is captured in a standardized fashion.
The Definition of Provider Credentialing Services
Provider credentialing services also serve the function of ensuring the accuracy of billing and documentation. The credentialing process is how providers are able to bill insurance companies for patient care. Evidence that correct CPT Code 92504 claims are incorrectly documented for auditory brainstem response services in other disciplines if the provider is not credentialed. Keeping current with your credentials can help you avoid delays in payment and streamline claims processing.
Conclusion
Proper coding for CPT Code 92504 is key to ensuring that your practice receives full reimbursement. Healthcare providers can help ensure that they are getting paid appropriately, and promptly, by including extensive information about the patient’s condition, the results of any tests performed and an explanation by a provider. Adding a medical billing team, taking on denial management services, and ensuring that provider credentialing services remain up to scratch all help in the minimising the gap.
Adhering to these best practices minimizes claim rejections, maximizes revenue, and enables healthcare providers to concentrate on providing patient care. How to Become a Better Medical Biller by Training Office Staff Proper Billing and Documentation This… accurate billing and documentation in medical Practice is not only just an administrative duty, but also requisite for the helpfulness of health related practice.




Comments are closed